COVID-19 accelerated a number of trends already brewing in the healthcare industry, and that’s not likely to change this year, according to a new report from CVS Health.
The healthcare giant released its annual Health Trends Report on Tuesday, and the analysis projects several industry trends that are likely to define 2021 in healthcare, ranging from technology to behavioral health to affordability.
“We are facing a challenging time, but also one of great hope and promise,” CVS CEO Karen Lynch said in the report. “As the pandemic eventually passes, its lessons will serve to make our health system more agile and more responsive to the needs of consumers.”
Here’s a look at four of CVS’ predictions:
1. A looming mental health crisis
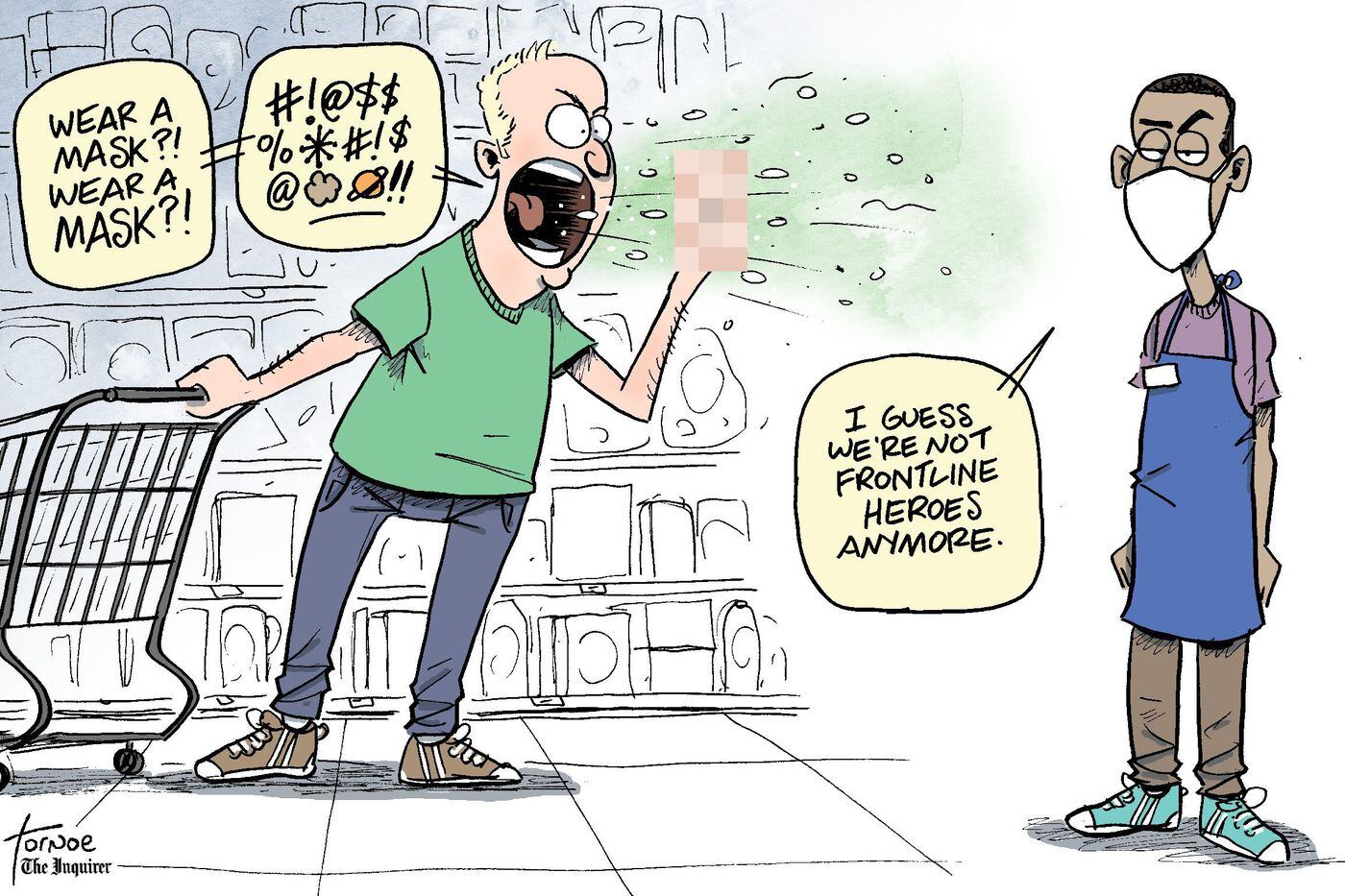
Behavioral health needs were a significant challenge in healthcare prior to COVID-19, but the number of people reporting declining mental health jumped under the pandemic.
Cara McNulty, president of Aetna Behavioral Health, said in a video attached to the report that it will be critical to “continue the conversation around mental health and well-being” as we emerge from the pandemic and to reduce stigma so people who need help seek it out.
“We’re normalizing that it’s important to take care of our mental well-being,” she said.
Data released in December by GoodRx found that prescription fills for depression and anxiety medications hit an all-time high in 2020. GoodRx researchers polled 1,000 people with behavioral health conditions on how they were navigating the pandemic, and 63% said their depression and/or anxiety symptoms worsened.
McNulty said symptoms to look for when assessing whether someone is struggling with declining mental health include whether they’re withdrawn or agitated or if there’s a notable difference in their self-care routine.
2. Pharmacists take center stage
CVS dubbed 2021 “the year of the pharmacist” in its report.
The company expects pharmacists to be a key player in a number of areas, especially in vaccine distribution as that process inches toward broader access. They also offer a key touchpoint to counsel patients about their care and direct them to appropriate services, CVS said.
CVS executives said in the report that they see a significant opportunity for pharmacists to have a positive impact on the social determinants of health.
“We’ve found people are not only open and willing to share social needs with their pharmacists but in many cases, they listen to and act on the advice and recommendations of pharmacists,” Peter Simmons, vice president of transformation, pharmacy delivery and innovation at CVS Health, said in the report.
3. Finding ways to mitigate the cost of high-price therapies
Revolutionary drugs and therapies are coming to market with eye-popping price tags; it’s not uncommon to see new pharmaceuticals priced at $1 million or more. For pharmacy benefit managers, this poses a major cost challenge.
To address those prices, CVS expects value-based contracting to take off in a big way. And drugmakers are comfortable with the idea, according to the report. Novartis, for example, is offering insurers a five-year payment plan for its $2 million gene therapy Zolgensma, with refunds available if the drug doesn’t achieve desired results.
CVS said the potential for these therapies is clear, but many payers want to see some type of results before they fork over hundreds of thousands.
“Though the drug may promise to cure these patients for life, these are early days in their use,” said Joanne Armstrong, M.D., enterprise head of women’s health and genomics at CVS Health, in the report. “What we’re saying is, show us the clinical value proposition first.”
CVS said it’s also offering a stop-loss program for gene therapy to self-funded employers contracted with Aetna and/or Caremark to assist them in capping the expenses associated with these drugs.
4. Getting into the community to address diabetes
Diabetes risk is higher among vulnerable populations, such as Black patients, and addressing it will require local and community-based solutions, CVS executives said in the report. Groups at the highest risk for the disease are less likely to live in areas with easy access to a supermarket, for example, which boosts their risk of unhealthy eating, according to the report.
The two key hurdles to addressing this issue are access and affordability. The rise in retail clinics and ambulatory care centers can get at the access issue, as they can offer a way to better meet patients where they are.
At CVS’ MinuteClinics, patients can walk in and receive a number of services to assist them in managing diabetes, including screenings, consultations with providers and connections to diabetes educators who can assist with lifestyle changes.
Retail locations can also assist with medication costs, creating a one-stop-shop experience that’s easier for many diabetes patients to slot into their daily lives, CVS said.
“Diabetes is a case study in how a more connected experience can translate to simpler, affordable and more accessible care for underserved communities,” said Dan Finke, executive vice president of CVS Health and president of its healthcare benefits division.