https://www.healthcaredive.com/news/retail-makes-its-case-telehealth-and-voice-tech-dominate-6-takeaways-from/566548/

Headlines at HLTH 2019 included a peek behind the curtain at the secretive healthcare division of tech giant Google from ex-Geisinger CEO David Feinberg, Uber’s newly inked deal with Cerner and a preventive health push by Facebook sparking renewed data privacy concerns.
On the government side, outgoing head of CMS’ innovation center Adam Boehler suggested industry will be pleased with his replacement and CMS Administrator Seema Verma promised further Medicaid deregulation and “humility” in government.
But the four-day conference last week also covered some broader themes, including retail’s presence in the industry, the rise of telehealth and voice tech and the challenges of interoperability. Here are six of the biggest takeaways from Las Vegas.
Retail still defining its role in healthcare
Executives from Walmart and CVS taking to the main stage at HLTH to tout their initiatives.
Walmart’s VP of transformation, Marcus Osborne, talked up the company’s first health superstore in Dallas, Georgia, which opened this fall. The center provide patients with primary care, dental care, vision care and psychiatric and behavioral health counseling, with the goal of providing an integrated healthcare experience in the traditionally underserved area. Lab services and imaging are available on-site, as are nutrition and fitness classes.
“When you give consumers options, they engage more,” Osborne said. “The healthcare system is designed to be complex when it should be simple.”
A primary care visit at Walmart Health Center costs a flat fee of $40. For an adult, getting a dental checkup and cleaning costs $50, and an eye appointment is $45. Therapy services are $1 per minute.
The store pits the Bentonville, Arkansas-based retailer directly against CVS Health, which is expanding its own health-focused clinics, called HealthHUBs, to 13 new markets by the end of next year.
Brick-and-mortar behemoths’ attempts to position themselves as the front door to healthcare are spurred by the increasing push of consumerism in healthcare.
“With the emergence of this retail health consumer, we’ve got to make healthcare more integrated than it’s been for several years now,” CVS CEO Larry Merlo said.
Limits of consumerism
But engagement is notoriously tricky, and consumerism can only take the industry so far. Healthcare startups providing a new way of accessing or managing care, like digital chat startups allowing consumers to talk via text with a remote physician or chronic care management companies, are struggling to establish trust with the consumer.
Hank Schlissberg, president of care manager Vively Health, a subsidiary of DaVita that assumes full risk for its population, compared the sea change in the industry to what’s happened with companies like AirBnB.
“I sleep in someone else’s bed. I shower in their shower. And we’ve convinced ourselves that’s totally normal,” he said. “All I want to do is provide people with free healthcare. And convincing people of that is much harder than we expected.”
Natalie Schneider, VP of Digital Health for Samsung, agreed, telling Healthcare Dive consumers are “routinely irrational” and don’t act in their own best interests. But “we’re seeing policyholders, health plans and others in healthcare not only account for this irrationality, but also capitalize on it” through incentives like providing a reward immediately following a healthy behavior.
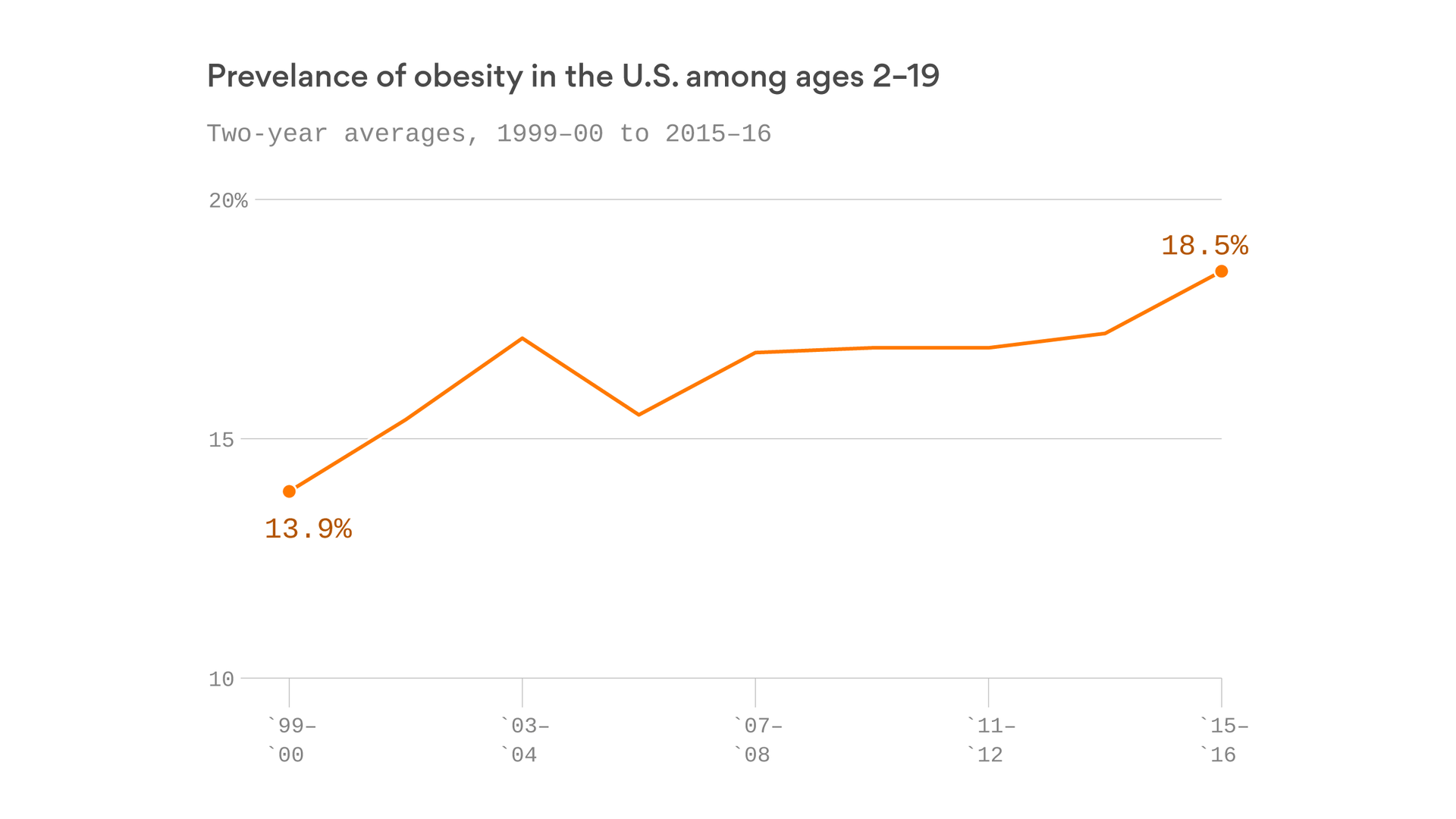
The wearables trend is a key example, experts said. Payers and providers alike are increasingly turning to the tech in an effort to engage consumers in wellness, fitness and preventive care activities. However, the ROI of trackers, whether from Apple Watch, Fitbit, Samsung or others, is still unproven.
“We’ve seen a lot of technologies and they’re often not that smart and very rarely wearable,” Tom Waller, who heads up the R&D lab of athleisure retailer lululemon, said. “We’re still patiently waiting for that perfect contextualization of data that will give us both a physical and emotional insight, and that we can use to augment an existing behavior to nudge someone in the right way.”
“At the end of the day, these patients are consumers, and consumers have been trained over the last 10 years to decide what quality they want, to decide when they want it and how they want to get it,” Robbie Cape, CEO of primary care startup 98point6, said. “Healthcare hasn’t caught up to that.”
Execution could stymie looming interoperability rules
Two rules to halt information blocking from HHS are expected to be finalized any day now. Despite the regulatory pressure, industry is “still a ways from true interoperability,” said Ed Simcox, CTO and acting CIO of HHS, due to a slew of factors like a lack of economic incentive for EHR vendors.
The rules would impose a slate of new requirements on healthcare companies. Payers in federal programs would have to provide their 125 million patients with free electronic access to their personal health data by the end of next year; healthcare companies would have to adopt standardized application programming interfaces allowing their disparate software systems to communicate; and any player found information blocking could be fined up to $1 million per violation.
Google Cloud’s director of global healthcare solutions, Aashima Gupta, warned that although the government might mandate new standards, that doesn’t mean industry will be able or willing to immediately adhere to them.
Additionally, the government is still playing catch-up to technology, and interoperability is no different, Pranay Kapadia, CEO of voice-enabled digital assistant Notable, told Healthcare Dive. The rules are the “right thing to do, and then there’ll be an evolution of it, and then there’ll be another evolution of it.”
”This problem is much bigger than big tech or government or health systems or innovators,” Gupta said. “It’s an ecosystem problem. No player can do it alone.”
Despite the private sector’s uncertainly, Don Rucker, the head of the Office of the National Coordinator for Health IT, said interoperability had fostered price and business model transparency in every other U.S. industry over the past few decades.
“Healthcare is just about the last one to resist,” Rucker said. “I don’t think that will be much longer.”
Telehealth and voice tech: the belles of the ball
Telehealth was unsurprisingly a big focus at HLTH, with themes touching on expansion to complex care needs, followup visits and chronic care management and barriers like state physician licensure.
It’s an “efficiency mechanism” that can help a lot in areas like primary care, Teladoc COO David Sides told Healthcare Dive.
Voice-enabled tech was another focus of chatter in Las Vegas. The technology, which allows physicians free use of their hands while enabling them to take notes or write a script, for example, is currently experiencing heavy hype from industry and Silicon Valley as a way to streamline the heavy EHR and documentation requirements on physicians.
Talking is an “important element to how people interface with things,” Notable’s Kapadia said. “You have to think of things from a human perspective.”
Suki also announced at HLTH it expanded its relationship with Google’s cloud computing business. The digital assistant’s CEO, Punit Soni, told Healthcare Dive industry could expect to hear about two “very, very large deployment announcements” with health systems in the near future as providers become more comfortable levering the software to cut down documentation time for clinicians.
Solving for social determinants, preventive health
A slew of players rolled out initiatives targeting social determinants of health in Las Vegas.
Uber Health is now available for providers to schedule non-emergency rides for their patients via Cerner’s EHR platform in a bid to provide better access to transportation for underserved populations. The one-year-old NEMT division of San Francisco-based Uber has roughly 1,000 partnerships across payers, healthcare tech companies and providers such as Boston Medical Center.
“You need to develop a benefit that serves the needs of your distinct population,” Jami Snyder, director of Arizona’s Medicaid and CHIP programs, said. The state recently partnered with ride-hailing company and Uber rival Lyft to provide rides for eligible Medicaid beneficiaries.
Kaiser Permanente rolled out a food insecurity initiative to connect eligible California residents with CalFresh, the state’s supplemental nutrition assistance or food stamp program. The integrated, nonprofit health system plans to reach out via text and mail to more than 600,000 Kaiser Permanente health plan members with a goal of getting 100,000 enrolled in CalFresh by spring 2020.
If the program is successful, Kaiser plans to expand it to the rest of the country, CEO Bernard Tyson, noting “healthcare across the ecosystem of health plays a very small part” in outcomes. “Things like behavior, genetics and where you live has a bigger impact.”
On the preventive health side, Facebook launched a consumer health tool. Users plug in their age and sex in return for targeted heart, cancer and flu prevention measures, with information supplied by healthcare groups like the American Cancer Society.
The pilot for the $7 billion tech behemoth will be evaluated for six months to a year before being expanded to other preventable conditions to make consumers their “own health advocates,” Freddy Abnousi, Facebook’s head of health research, said. “The lion’s share of health outcomes is driven by social and behavioral variables.”
CVS is similarly working to combat SDOH factors by leveraging its reams of consumer data, Firdaus Bhathena, the retail pharmacy giant’s CDO, told Healthcare Dive. If someone doesn’t pick up their prescription, “there’s a number of ways we can engage with them,” including by text message or speaking to services in the local town, to see if transportation to the pharmacy, a lack of funds or some other issue is stopping the person from receiving the medication they need.
Funding disruption
Much of the industry runs today like non-healthcare companies ran 50 or 60 years ago, according to entrepreneur Mark Cuban.
“For that reason, they’re ripe for disruption,” Cuban said at HLTH.
Investors and startups alike are taking note. Venture capitalists, eager to fund new medical solutions and methods of care delivery, pumped $26.3 billion into more than 1,500 healthcare startups in just the first 10 months of 2018.
Providers looking to invest in new solutions or acquire startups are looking for a relatively mature corporate structure and an alignment with existing priorities in-house, according to Dan Nigrin, SVP and CIO at Boston Children’s Hospital.
“It starts with our organizational strategy,” agreed Rebecca Kaul, VP at the MD Anderson Cancer Center. An attractive startup presents “something that really drives change,” she said. “If you’re pitching a solution that isn’t at a given time part of our strategy, it may not be the right time for us to connect.”
Highmark Health CEO David Holmberg told Healthcare Dive its physicians lead system-wide conversations in what areas need investment. “Ultimately, that’s how you’ll get things to scale.”
Intermountain Healthcare is similarly interested in ways to manage and inject value into its operations. “We’re not interested in point solutions,” Dan Liljenquist, SVP of the Salt Lake City-based nonprofit provider said, adding he deletes and blocks emailed pitches he receives. “We’re interested in technologies that obviate the need for clinical interventions, that help people solve their own problems, and the way to do that is not a point solution but in a systemic, creative way.”
Payers have similar priorities and seek out companies to invest in that could provide value down the road. Cigna Ventures, which recently invested in precision medicine company GNS Healthcare, looks for new tools across the areas of insight and analytics, digital health and retail and all-around care delivery and enablement, for example.
“We’re looking for companies that are innovative and looking to solve important problems,” Tom Richards, global strategy and business development leader at Cigna, told Healthcare Dive, noting most companies start with a more focused solution and then expand.
For example, chronic disease platform Omada Health, which raised $50 million in a 2017 funding round led by Cigna Ventures, started with diabetes, but has since expanded its care management services to hypertension, Type 2 diabetes and behavioral and mental health.