The Taylor Swift ticketing debacle of 2022 left thousands of frustrated ‘Swifties’ without a chance to see their favorite artist in concert. And it also highlighted the trouble that arises when companies like Ticketmaster gain monopolistic control.
In any industry, market consolidation limits competition, choice and access to goods and services, all of which drive up prices.
But there’s another—often overlooked—consequence.
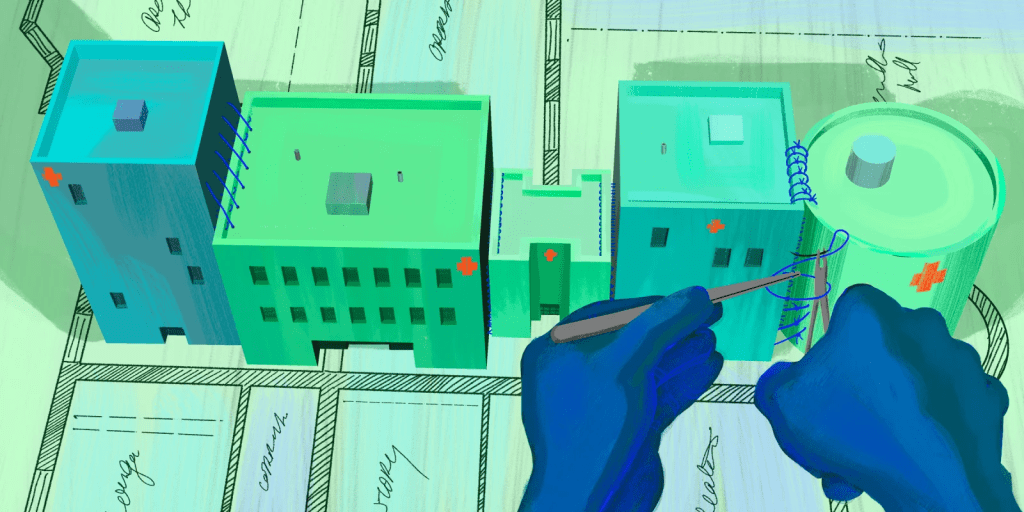
Market leaders that grow too powerful become complacent. And, when that happens, innovation dies. Healthcare offers a prime example.
And industry of monopolies
De facto monopolies abound in almost every healthcare sector: Hospitals and health systems, drug and device manufacturers, and doctors backed by private equity. The result is that U.S. healthcare has become a conglomerate of monopolies.
For two decades, this intense concentration of power has inflicted harm on patients, communities and the health of the nation. For most of the 21st century, medical costs have risen faster than overall inflation, America’s life expectancy (and overall health) has stagnated, and the pace of innovation has slowed to a crawl.
This article, the first in a series about the ominous and omnipresent monopolies of healthcare, focuses on how merged hospitals and powerful health systems have raised the price, lowered the quality and decreased the convenience of American medicine.
Future articles will look at drug companies who wield unfettered pricing power, coalitions of specialist physicians who gain monopolistic leverage, and the payers (businesses, insurers and the government) who tolerate market consolidation. The series will conclude with a look at who stands the best chance of shattering this conglomerate of monopolies and bringing innovation back to healthcare.
How hospitals consolidate power
The hospital industry is now home to a pair of seemingly contradictory trends. On one hand, economic losses in recent years have resulted in record rates of hospital (and hospital service) closures. On the other hand, the overall market size, value and revenue of U.S. hospitals are growing.
This is no incongruity. It’s what happens when hospitals and health systems merge and eliminate competition in communities.
Today, the 40 largest health systems own 2,073 hospitals, roughly one-third of all emergency and acute-care facilities in the United States. The top 10 health systems own a sixth of all hospitals and combine for $226.7 billion in net patient revenues.
Though the Federal Trade Commission and the Antitrust Division of the DOJ are charged with enforcing antitrust laws in healthcare markets and preventing anticompetitive conduct, legal loopholes and intense lobbying continue to spur hospital consolidation. Rarely are hospital M&A requests denied or even challenged.
The ills of hospital consolidation
The rapid and recent increase in hospital consolidation has left hundreds of communities with only one option for inpatient care.
But the lack of choice is only one of the downsides.
Hospital administrators know that state and federal statutes require insurers and self-funded businesses to provide hospital care within 15 miles of (or 30 minutes from) a member’s home or work. And they understand that insurers must accept their pricing demands if they want to sell policies in these consolidated markets. As a result, studies confirm that hospital prices and profits are higher in uncompetitive geographies.
These elevated prices negatively impact the pocketbooks of patients and force local governments (which must balance their budgets) to redirect funds toward hospitals and away from local police, schools and infrastructure projects.
Perhaps most concerning of all is the lack of quality improvement following hospital consolidation. Contrary to what administrators claim, clinical outcomes for patients are no better in consolidated locations than in competitive ones—despite significantly higher costs.
How hospitals could innovate (and why they don’t)
Hospital care in the United States accounts for more than 30% of total medical expenses (about $1.5 trillion). Even though fewer patients are being admitted each year, these costs continue to rise at a feverish pace.
If our nation wants to improve medical outcomes and make healthcare more affordable, a great place to start would be to innovate care-delivery in our country’s hospitals.
To illuminate what’s possible, below are three practical innovations that would simultaneously improve clinical outcomes and lower costs. And yet, despite the massive benefits for patients, few hospital-system administrators appear willing to embrace these changes.
Innovation 1: Leveraging economies of scale
In most industries, bigger is better because size equals cost savings. This advantage is known as economies of scale.
Ostensibly, when bigger hospitals acquire smaller ones, they gain negotiating power—along with plenty of opportunities to eliminate redundancies. These factors could and should result in lower prices for medical care.
Instead, when hospitals merge, the inefficiencies of both the acquirer and the acquired usually persist. Rather than closing small, ineffective clinical services, the newly expanded hospital system keeps them open. That’s because hospital administrators prefer to raise prices and keep people happy rather than undergo the painstaking process of becoming more efficient.
The result isn’t just higher healthcare costs, but also missed opportunities to improve quality.
Following M&A, health systems continue to schedule orthopedic, cardiac and neurosurgical procedures across multiple low-volume hospitals. They’d be better off creating centers of excellence and doing all total joint replacements, heart surgeries and neurosurgical procedures in a single hospital or placing each of the three specialties in a different one. Doing so would increase the case volumes for surgeons and operative teams in that specialty, augmenting their experience and expertise—leading to better outcomes for patients.
But hospital administrators bristle at the idea, fearing pushback from communities where these services close.
Innovation 2: Switching to a seven-day hospital
When patients are admitted on a Friday night, rather than a Monday or Tuesday night, they spend on average an extra day in the hospital.
This delay occurs because hospitals cut back services on weekends and, therefore, frequently postpone non-emergent procedures until Monday. For patients, this extra day in the hospital is costly, inconvenient and risky. The longer the patient stays admitted, the greater the odds of experiencing a hospital acquired infection, medical error or complications from underlying disease.
It would be possible for physicians and staff to spread the work over seven days, thus eliminating delays in care. By having the necessary, qualified staff present seven days a week, inpatients could get essential, but non-emergent treatments on weekends without delay. They could also receive sophisticated diagnostic tests and undergo procedures soon after admission, every day of the week. As a result, patients would get better sooner with fewer total inpatient days and far lower costs.
Hospital administrators don’t make the change because they worry it would upset the doctors and nurses who prefer to work weekdays, not weekends.
Innovation 3: Bringing hospitals into homes
During Covid-19, hospitals quickly ran out of staffed beds. Patients were sent home on intravenous medications with monitoring devices and brief nurse visits when needed.
Clinical outcomes were equivalent to (and often better than) the current inpatient care and costs were markedly less.
Building on this success, hospitals could expand this approach with readily available technologies.
Whereas doctors and nurses today check on hospitalized patients intermittently, a team of clinicians set up in centralized location could monitor hundreds of patients (in their homes) around the clock.
By sending patients home with devices that continuously measure blood pressure, pulse and blood oxygenation—along with digital scales that can calibrate fluctuations in a patient’s weight, indicating either dehydration or excess fluid retention—patients can recuperate from the comforts of home. And when family members have questions or concerns, they can obtain assistance and advice through video.
Despite dozens of advantages, use of the “hospital at home” model is receding now that Covid-19 has waned.
That’s because hospital CEOs and CFOs are paid to fill beds in their brick-and-mortar facilities. And so, unless their facilities are full, they prefer that doctors and nurses treat patients in a hospital bed rather than in people’s own homes.
Opportunities for hospital innovations abound. These three are just a few of many changes that could transform medical care. Instead of taking advantage of them, hospital administrators continue to construct expensive new buildings, add beds and raise prices.