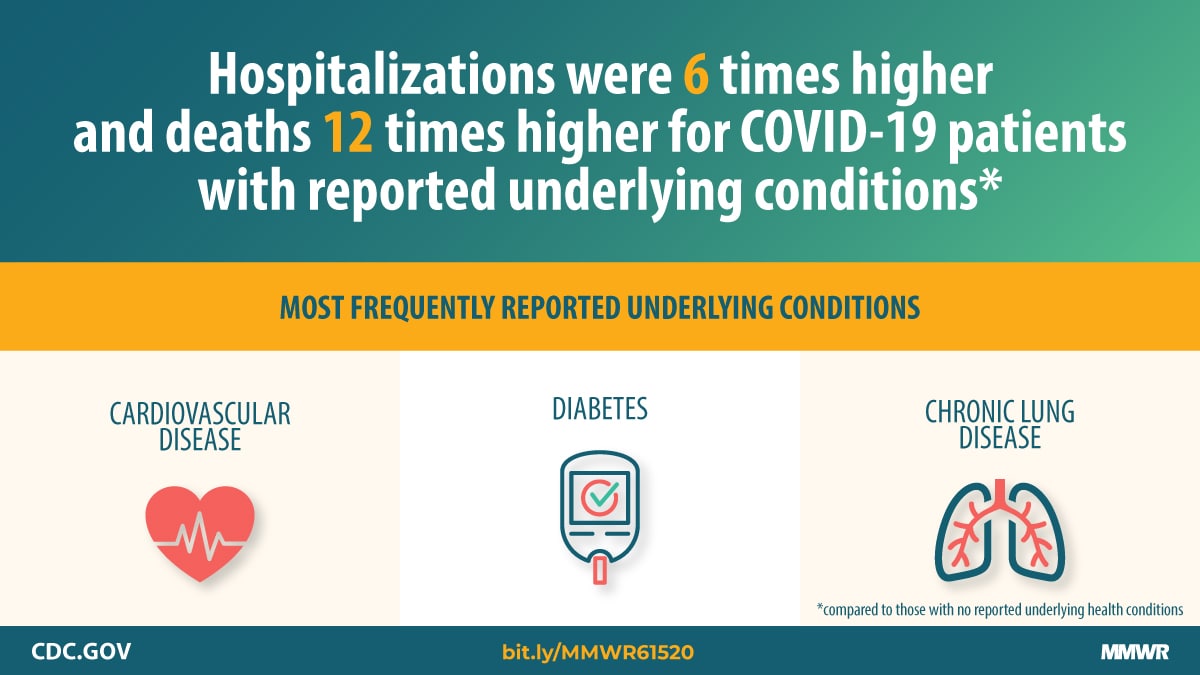
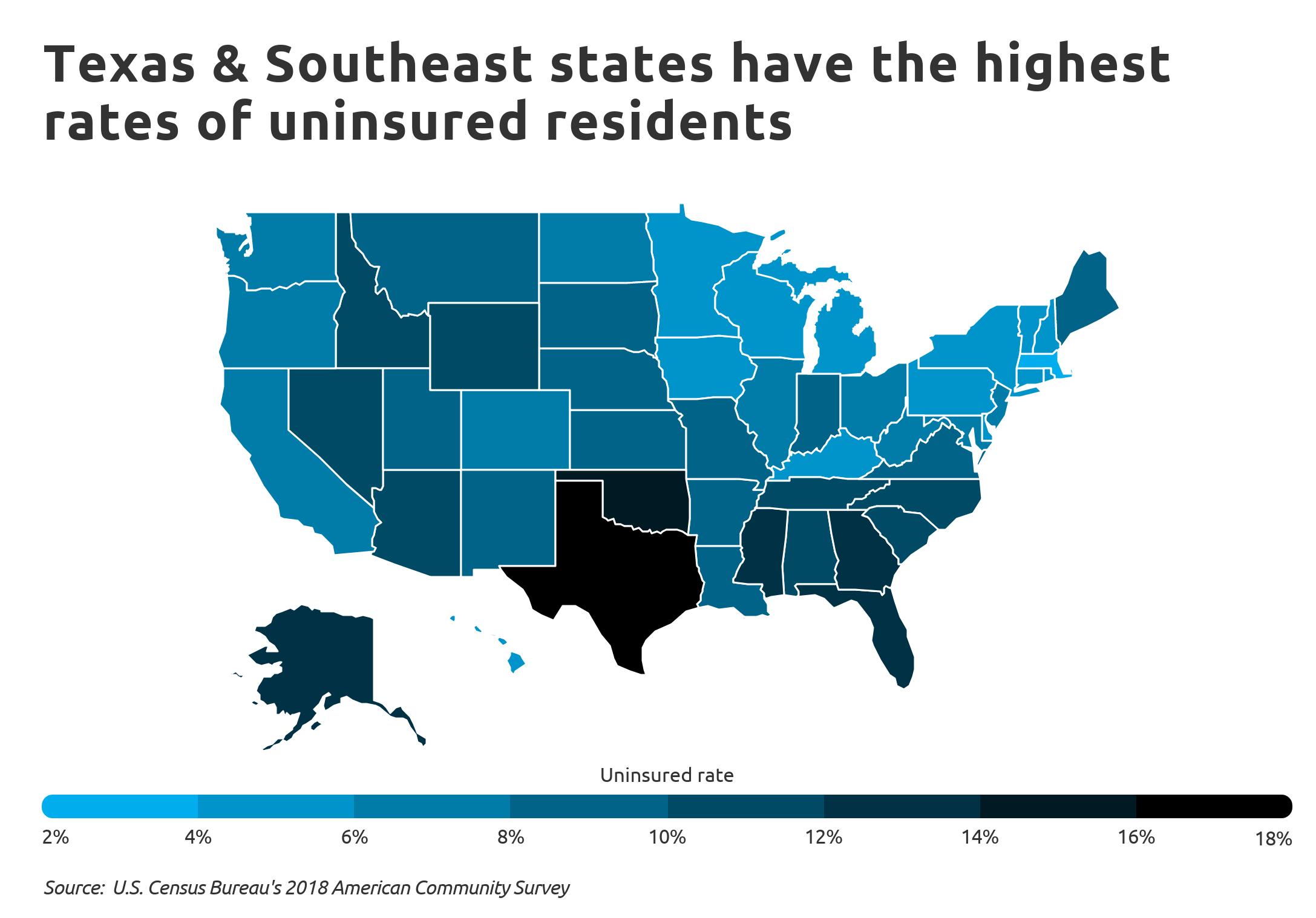
The coronavirus pandemic hit the nation hard and fast, infecting Americans from coast to coast, overwhelming health care systems and wreaking havoc on the economy. Those with pre-existing conditions – like diabetes and cardiovascular disease – are more vulnerable to the deadly virus. Americans have higher rates of these chronic conditions than other countries, in part because so many people live without health insurance or have shoddy coverage. This has become increasingly worse over the last four years as underlying health coverage has shrunken for the virus’s hardest hit victims: Black Americans, Native Americans and people of color.
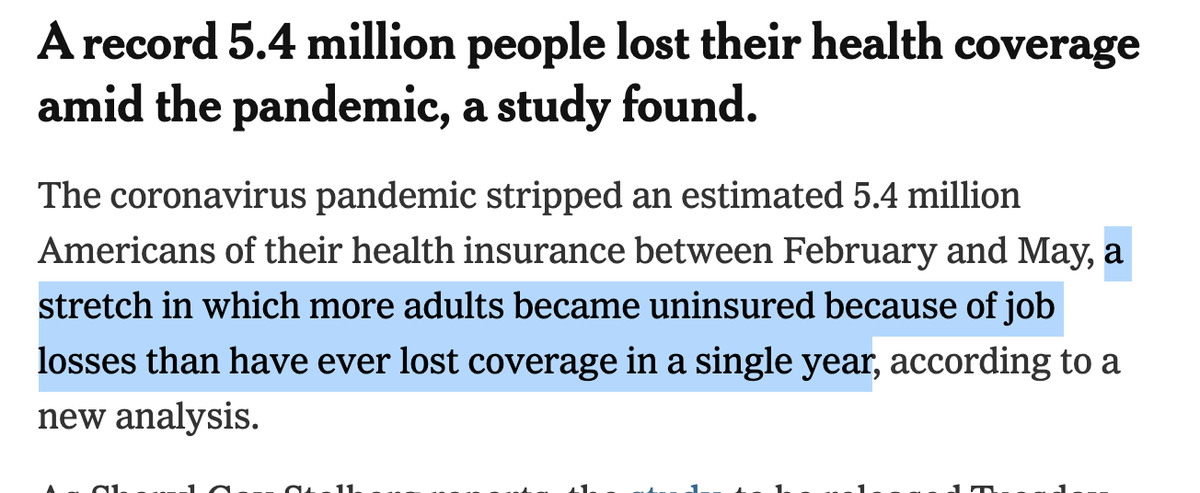
Of the hundreds of thousands of Americans now recovering from COVID-19, many will undoubtedly have new chronic conditions, like lasting lung damage. This will be on top of the pre-existing conditions many who were predisposed to coronavirus already had. Record job losses in the wake of the pandemic have resulted in the loss of employer-sponsored coverage for more than 5 million Americans who are now on the hunt for new, affordable health insurance plans.
This presents the perfect storm for junk insurance plans – short-term limited duration insurance plans – that allow discrimination based on pre-existing conditions, expose consumers to financial risk and provide inadequate coverage. STLDIs are more dangerous now than ever in our new COVID-19 reality. Let’s be clear: These junk insurance plans – touted by the Trump administration and supported through taxpayer dollars – are not the answer. It is time for our leaders to put back the limitations on how long they can be used.
As their name suggests, short-term limited duration plans are meant to be used temporarily to bridge short-term gaps in coverage that arise from a job loss or other extenuating circumstance. However, new federal rules under the Trump administration have allowed the coverage period of STLDI plans to expand from six to 12 months. The administration has also promoted these plans to states as being eligible for federal subsidies, meaning our tax dollars help pay for them. President Donald Trump himself has touted these plans for being more affordable than Obamacare, but that is because they lack the same protections and do not meet minimum essential coverage standards under the law.
That is what makes these plans so dangerous. Though they tend to be less expensive than Affordable Care Act plans, they leave consumers vulnerable to unanticipated out-of-pocket costs by offering bare-bones coverage. Unlike ACA plans, STLDI plans can exclude coverage for pre-existing conditions, do not cover the cost of prescription drugs, have annual or lifetime maximums on covered services, and are not required to cover preventive services like cancer screenings or maternity care.
The lower price tag may lure consumers suffering financially during the pandemic, but they are high risk for those who do not fully understand what they are buying. Without carefully reading the fine print, many may not know before purchasing that STLDI plans are exempt from ACA rules as well as regulations for insurers recently passed in the Families First Coronavirus Response Act and the Coronavirus Aid, Relief, and Economic Security Act. We have already seen the pandemic exacerbate existing health inequalities in America, and now these plans expose consumers, especially low-income individuals and those with chronic conditions, to more discrimination and financial ruin.
The Department of Health and Human Services has already acknowledged that these plans fall short. In fact, the government is having to cover the cost of COVID-19 testing for people with STLDI plans, classifying them as “uninsured.” Yet, they will not cover the cost of COVID-19 treatment, meaning those with STLDI plans could face bills in the thousands of dollars, considering the average cost to treat a hospitalized coronavirus patient is $30,000.
Consumers for Quality Care, a coalition of advocates and former policy makers which provides a voice for patients in the health care debate, recently sent a letter to HHS Secretary Alex Azar and Centers for Medicare & Medicaid Services Administrator Seema Verma asking that they protect consumers from these dangerous plans.
This pandemic has laid bare how dangerously unprepared America’s health care system is for a large-scale public health crisis. People needed high-quality insurance coverage before coronavirus hit, and they will need it long after the pandemic subsides. Let this be a lesson to the Trump administration – it is time to stop backing junk insurance plans and remove them from the open market. If our leaders fail to act, the lives and financial well-being of millions of Americans are at stake.